 Introduction:
Introduction:
Multi-slice or multi-detector row CT scanners, capable of imaging four simultaneous, parallel slices in a single rotation, were first introduced in 1998. Since then, scanners with 6, 8, 10 and 16 slice capabilities have become available and have made a marked impact on the role of CT in the diagnostic radiology department. Most recently 32, 40 and 64 slice scanners have been announced and the trend for increased capabilities and hence extended applications of CT is certain to continue.
 CT scanning has been recognised as a high radiation dose modality, when compared to other diagnostic X-ray techniques, since its launch into clinical practice more than 30 years ago. Over that time, as scanner technology has developed and its use has become more widespread, concerns over patient radiation doses from CT have grown [1, 2]. The introduction of multi-slice scanners has focussed further attention on this issue, and it is generally believed that it will lead to higher patient doses [3].
CT scanning has been recognised as a high radiation dose modality, when compared to other diagnostic X-ray techniques, since its launch into clinical practice more than 30 years ago. Over that time, as scanner technology has developed and its use has become more widespread, concerns over patient radiation doses from CT have grown [1, 2]. The introduction of multi-slice scanners has focussed further attention on this issue, and it is generally believed that it will lead to higher patient doses [3].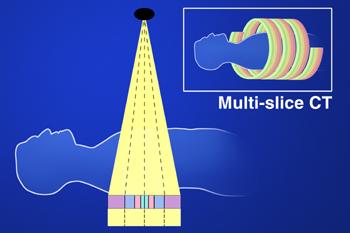
The amount of radiation dose a patient receives from a CT scan depends upon two key factors, the design of the scanner and also on the way that the scanner is used. The designs of single slice and multi-slice scanners are similar in most aspects that affect radiation dose, but multi-slice scanning can potentially result in higher radiation risk to the patient due to increased capabilities allowing long scan lengths at high tube currents.
The aim of this leaflet is to explain how the differences between single and multi-slice systems will impact on patient doses. The term ‘dose’ is used here in its broad context and, unless otherwise stated, generally refers to both absorbed dose and effective dose.
The leaflet also includes a description of the principles of automatic tube current control systems available on modern scanners. Although not exclusive to multi-slice, they are now an integral part of most of these systems, and their development has progressed significantly alongside them.

